IT’S TIME TO TAKE CONTROL DON’T WAIT
Take the right steps to put your health first.
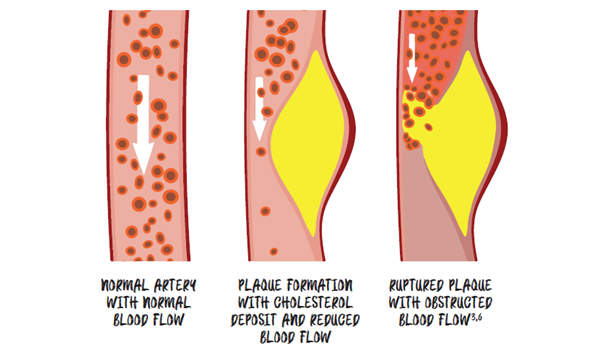
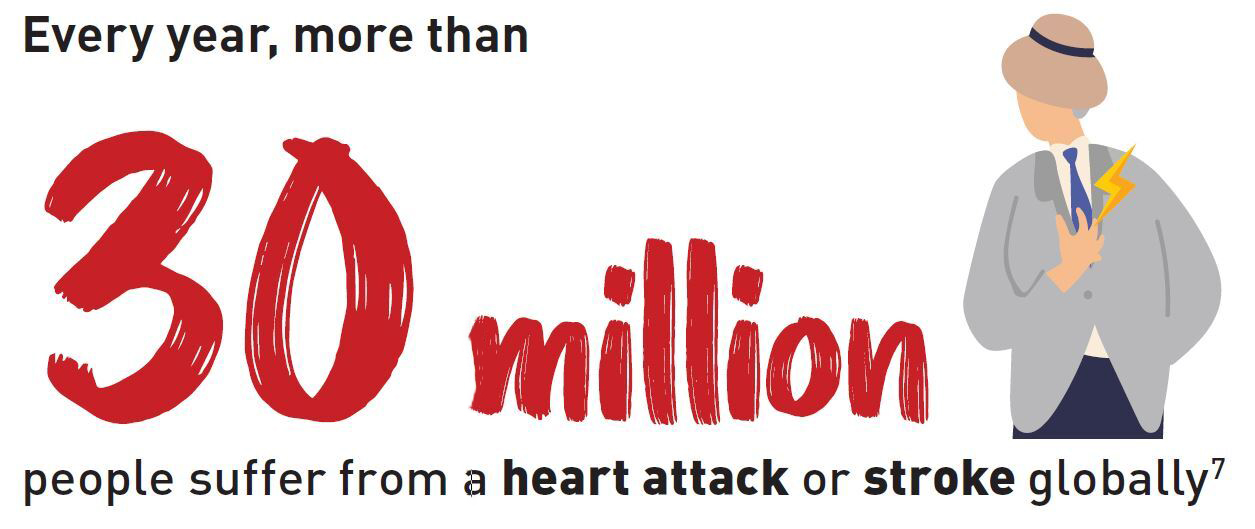
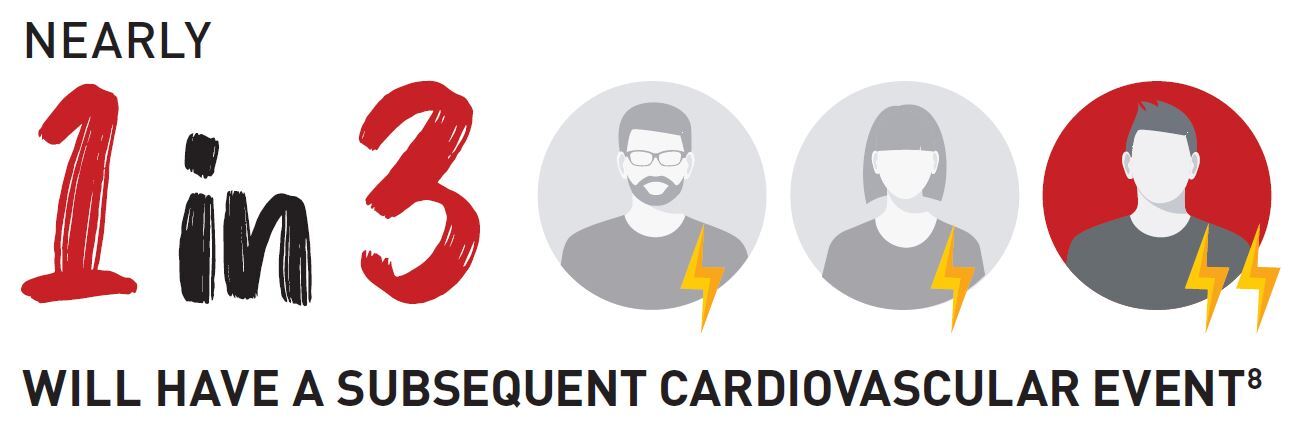
Schedule an appointment with your doctor to discuss your cholesterol level. If your numbers are too high despite being on a cholesterol-lowering therapy, talk to your doctor about treatment options that can further lower your cholesterol and risk of another heart attack or stroke.11 Be in control of your health, fully engage in life and reduce the hidden risk of heart attack or stroke.